112 new cases, 30 in hospital; Guam seeking FEMA's assistance for medical reinforcement
- By Johanna Salinas
- Aug 27, 2020
- 4 min read

The latest batch of Covid-19 test results showed 112 new cases, as the government scrambles to allocate more spaces to accommodate the surge of hospitalization.
As of Thursday night, the number of Covid-19 related patients admitted into the understaffed Guam Memorial Hospital has climbed to 30. The death toll is now 10.
The 112 new cases account for more than 10 percent of 1,002 samples tested.
The outbreak in the military is worsening as well, with a new total of 183. To date, there have been a total of 1,232 confirmed cases of Covid-19, 456 not in isolation, and 766 cases in active isolation.
The government is seeking to pool the island’s health care resources to beef up the limited nursing staff at GMH.
“We’ve been preparing from the very beginning for a surge like this and we’ve been covering all the bases,” Gov. Lou Leon Guerrero said. “This increase of cases is overtaxing.”
The governor said her administration has requested the Federal Emergency Management Agency and the U.S. Navy for medical backup.
“I understand that there are requests for ICU nurses and there are requests for some doctors also and respiratory therapists. That request has been sent in to FEMA and FEMA has moved it on up to the higher ups,” Leon Guerrero said.
She said the Joint Region Marianas commander, Adm. John Menoni, “is also on his side running it up to his chain of command.”
Defense Secretary Mark Esper will be on Guam Friday to meet with the Surgeon Cell to discuss staffing needs of Guam, the governor said.
GMH administrator Lillian Posadas discussed the bed reallocation at the hospital, increasing ICU beds to 17.
“In the 14-bed second floor ICU/CCU area, we created a partition separating non-Covid ICU and Covid ICU. In doing that, we added seven additional ICU beds for Covid patients. The advantage for having that is those beds have the capacity to do hemodialysis. That was one of our challenges,” said Posadas.
“In the Care 2 unit, which is just across the hallway, we have that Care 2 unit designated for an ICU bed for Covid patients.”
Originally, the plan was to have it for five patients, but because of the bulkiness of ventilators, it was capped at four.
GMH has 11 total beds for ICU patients. The third floor has an area that has six beds that can accommodate ICU care. “That is 17 beds for ICU patients,” she said. “We do have beds that can be for telemetry or regular medical patients. That’s a 26-bed area.”
The Skilled Nursing Unit in Barrigada Heights has the capacity for 54 beds. “The chiller we had, that’s been there for 25 years, we’ve been trying to get that replaced. We had it repaired and it is running, but it isn’t sufficiently keeping the facility cool,” said Posadas.
A contract to replace the AC is being reviewed by the AG office.
Posadas said the DPHSS has made requests with both the military and Guam Department of Education for staff assistance.
“We requested for 40 critical care nurses. We requested for critical care bathrooms,” said Posadas, who had a call with GDOE after the press conference. “We’ve requested to at least have 10 school nurses, because already some of them are helping DPHSS. There are about 18 to 20 of them.”
Posadas mentioned some private clinics willing to assign some of their nurses to the Guam Regional Medical City, so the private hospital can take in some Covid patients.
Posadas said she reached out to University of Guam student nurses for assistance, as well as GDOE school asides for maybe contact tracing or pushing patients in wheelchairs.
“The Guam Army National Guard will be assigning from their medical personnel about eight or 10 to come to the hospital to augment the nurses and the nursing team in the Covid care areas,” she said.
ADVERTISEMENT
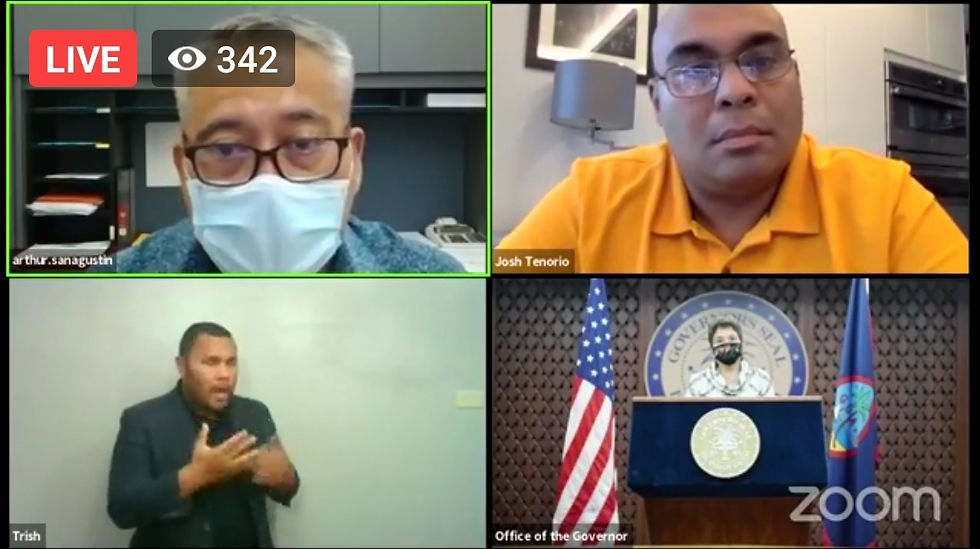
DPHSS has shifted from mass testing to target testing. “Our last specimens have significantly decreased from our Aug. 15 mass testing in which we had over 1,400 specimens drawn in one day,” DPHSS director Arthur San Agustin said.
“What’s happening now is a multitude of things. Over at the Northern Regional Community Health Center, we have AVID ID machines there that we’re using for testing, so results there come out sooner than when they go to the DPHSS lab. We’re receiving daily specimens from various labs and clinics. We run those runs those at our DPHSS lab,” he said.
He said DPHSS has cleared the Aug. 15 testing in terms of all the specimens and has been sending out results.
“The release we’ve sent out was about a seven day turnaround time. Prior to the 1,400+ swabs occurred on Aug. 15, we were hitting 48 hours notification time,” he said.
Read related stories
Governor modifies lockdown order
Dr. Felix Cabrera, a member of the governor’s Physicians Advisory team, said the situation is not expected to get better anytime soon.
“When our mobility, 100 percent being baseline, if we drop below 80 percent and if we take that day and move it about 15 days, that’s when we hopefully see at least a peak or plateau of hospitalizations. We’re still in that 15-day period. That period will end around Sept. 4,” he said.
“In all likelihood, it’s going to start to rise before we start seeing it get better. As long as our morbidity stays below 80 percent, ideally below 60 percent.”
Cabrera also went on to defend Dr. Janna Manglona’s comments about people being “out of control.”
“Dr. Manglona feels like a lot of us physicians on island and healthcare workers,” he said.
“We feel frustrated that there isn’t appreciation for how fragile our system is. When people have a ‘me first’ mentality, and with my discussion with her one on one, she was very much discussing her frustration of the protestors who were protesting the governor’s orders.”







